English
-



BLOGS
- 2025DATE06 - 30Pulmonary function testing (PFT) plays an indispensable role in diagnosing and managing respiratory diseases such as asthma, chronic obstructive pulmonary disease (COPD), interstitial lung diseases, and recently, post-viral lung impairments caused by infections like COVID-19.Read More
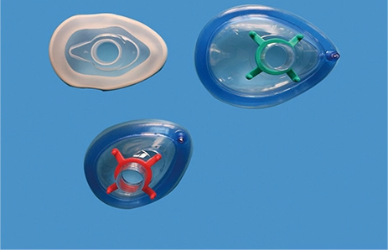
- 2025DATE06 - 25In the operating room (OR), the anesthesia mask is more than a simple conduit for delivering gases—it is the frontline barrier between sterile airway management and the surrounding environment. A reliable mask seal prevents anesthetic gas leaks that can expose staff to harmful waste gases, while simultaneously blocking pathogens from entering the patient's airway or escaping into the room.Read More
- 2025DATE06 - 19In the perioperative environment, anesthesia masks serve as the critical interface between patient and anesthetic delivery system. Yet, masks that fail to fit properly not only compromise ventilation efficacy and patient comfort but also heighten the risk of device-related contamination.Read More
- 2025DATE06 - 16Infection control is at the forefront of modern hospital practice, and nowhere is this more critical than in respiratory care. Oxygen delivery devices—ranging from simple nasal cannulas to advanced high-flow systems—are indispensable tools but also potential vectors for hospital-acquired infections (HAIs).Read More
- 2025DATE06 - 13Intravenous (IV) therapy is fundamental in healthcare, delivering fluids, medications, and nutrients directly into patients' bloodstream. Yet, IV therapy carries risks—particulate contamination, bacterial infection, and air embolism—that can have serious consequences. Infusion filters, small devices integrated into IV lines, serve as the critical last line of defense against these hazards.Read More
CONTACT US
NO.176, Gaoxin 5th Road, High-tech Industrial Park, Rizhao City276800, Shandong Province, China +86-13396234532 +86-13396234532Copyright © 2023 ZhenFu Group All Rights Reserved. Technology By leadong.com | Sitemap | Privacy Policy
-